本文主要是介绍肝移植笔记9 肝移植基础知识Discussion of liver transplantation-UCSF,希望对大家解决编程问题提供一定的参考价值,需要的开发者们随着小编来一起学习吧!
加州大学作者:
关于肝移植的讨论由移植外科医生Kayvan Roayaie,M.D.,Ph.D.和Sandy Feng,M.D.,Ph.D.撰写,冯博士是UCSF移植学院的现任成员,也是UCSF腹部移植奖学金计划的项目主任。Roayaie博士是UCSF移植部门的前研究员和临床讲师。
https://transplantsurgery.ucsf.edu/conditions--procedures/liver-transplant.aspx
收获总结
1.解剖学 (门静脉等)
2.功能 合成蛋白质, 分解有毒物质
3.肝损伤症状(黄疸, 腹水等)
4.MELD评分公式及影响指标
5.心源性死亡供体肝, 或活体供体移植可能增加并发症风险. (心源性死亡供体肝与原发性无功能或早期器官功能差、肝动脉血栓形成和胆道并发症的风险增加有关; 活体供体易发生肝动脉血栓)
6.肝移植手术的顺序
| 1.切口 2.评估腹部是否有异常导致无法进行肝移植(例如:未确诊的感染或恶性肿瘤) 3.切除原肝脏(解剖附着在腹腔的肝脏) 4.隔离重要结构(肝脏上方、后面和下方的下腔静脉;门静脉;胆总管;肝动脉) 5.切断上述结构和去除原患病的肝脏。(图7没找到) 6.缝合新肝脏:首先,通过连接供体和接受者的下腔静脉和门静脉来重新建立静脉血流。接下来,通过缝合供体和受体的肝动脉来重新建立动脉血流。最后,通过缝合供体和受体的胆总管来实现胆道引流。 7.确保充分控制出血 8.切口闭合 |
7.常见的5种肝移植并发症及其处理办法
目录
肝脏解剖学和功能
谁需要肝移植?
急性肝功能衰竭
慢性肝功能衰竭
失代偿性肝病的体征和症状
慢性肝损伤的原因
病毒性肝炎
酒精性肝病
代谢性肝病
自身免疫性肝病
遗传性肝病
血管性肝病
肝癌
谁不是肝移植的候选人
肝脏分配
梅尔德得分
地理和DSAs
器官捐献者的类型
脑死亡器官捐献者
心源性死亡器官捐献者
活体捐赠者
肝移植手术
手术并发症
免疫抑制
排斥反应
结果
肝脏解剖学和功能
Liver Anatomy and Function
肝脏具有许多关键功能,包括药物和毒素的代谢,去除正常身体代谢的降解产物(例如血液中氨和胆红素的清除),以及许多重要蛋白质和酶的合成(例如血液凝结所必需的因素)。
The liver serves many critical functions including metabolism of drugs and toxins, removing degradation products of normal body metabolism (for example clearance of ammonia and bilirubin from the blood), and synthesis of many important proteins and enzymes (such as factors necessary for blood to clot).
血液从肝动脉和门静脉两个通道进入肝脏,将营养和氧气带到肝细胞,也称为肝细胞和胆管。
Blood enters the liver from two channels, the hepatic artery and the portal vein, bringing nutrients and oxygen to liver cells, also known as hepatocytes, and bile ducts.
血液通过肝静脉离开肝脏,肝静脉流入下腔静脉,下腔静脉立即进入心脏。
Blood leaves the liver via the hepatic veins which drain into the inferior vena cava which immediately enters the heart.
肝脏产生胆汁,这是一种液体,有助于溶解脂肪,并通过肠道消除代谢废物和毒素。
The liver makes bile, a liquid that helps dissolve fat and eliminate metabolic waste and toxins via the intestine.
每个肝细胞产生胆汁并将其排泄到微观通道中,这些通道连接形成胆管。
Each hepatocyte creates bile and excretes it into microscopic channels that join to form bile ducts.
就像支流连接形成河流一样,胆管连接形成一个单一的“肝管”,将胆汁带入肠道。
Like tributaries joining to form a river, the bile ducts join to form a single "hepatic duct" that brings bile into the intestine.
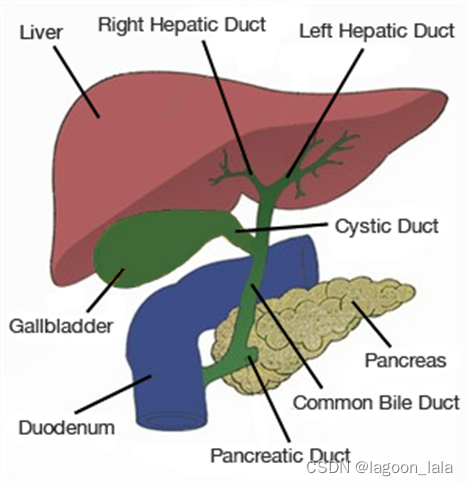
(注: Gallbladder 胆囊; Cystic Duct胆囊管; Common Bile Duct 胆总管; Pancreas 胰腺; Pancreatic Duct 胰管; Duodenum 十二指肠)
谁需要肝移植?
肝移植手术用正常和健康的肝脏代替衰竭或患病的肝脏。
Liver transplantation surgically replaces a failing or diseased liver with one that is normal and healthy.
此时,移植是治疗肝功能不全或肝功能衰竭的唯一方法,因为没有设备或机器能够可靠地执行肝脏的所有功能。需要肝移植的人通常有以下情况之一。
At this time, transplantation is the only cure for liver insufficiency or liver failure because no device or machine reliably performs all of the functions of the liver. People who require liver transplants typically have one of the following conditions.
急性肝功能衰竭
Acute Liver Failure
急性肝功能衰竭,也称为暴发性肝功能衰竭,当先前健康的肝脏遭受大量损伤导致肝功能不全的临床体征和症状时,就会发生。任何数量的事情都可能导致急性肝功能衰竭,但最常见的原因是对乙酰氨基酚(泰诺®)过量,病毒感染(已知或未知的病毒),摄入毒素如有毒蘑菇,或特异质药物反应。
Acute liver failure, also known as fulminant hepatic failure, occurs when a previously healthy liver suffers massive injury resulting in clinical signs and symptoms of liver insufficiency. Any number of things can lead to acute liver failure but the most common causes are acetaminophen (Tylenol®) overdose, viral infections (known or yet unknown virus), ingestion of a toxin such as poisonous mushrooms, or an idiosyncratic drug reaction.
这种情况的标志是在皮肤发黄(黄疸)发作后八周内发生意识模糊(脑病)。
The hallmark of this condition is the development of confusion (encephalopathy) within eight weeks after the onset of yellowing of the skin (jaundice).
出现意识模糊的原因是通常由肝脏代谢的毒素会积聚。
Confusion occurs because toxins typically metabolized by the liver accumulate.
与慢性肝病患者不同,慢性肝病患者在等待肝移植时可以存活数周至数月至数年,急性肝功能衰竭患者如果不移植,可能会在几天内死亡。这些患者被列为最高优先级(状态I),将他们置于捐赠者肝脏的地方/区域和国家等待名单的顶部。
Unlike patients with chronic liver disease, who can survive weeks to months to years while awaiting liver transplantation, patients with acute liver failure may die within days if not transplanted. These patients are listed at highest priority (Status I), placing them at the top of local, regional and national waiting lists for a donor liver.
慢性肝功能衰竭
Chronic liver failure
肝脏具有显着的自我修复能力,以应对损伤。
The liver has a remarkable ability to repair itself in response to injury.
然而,反复的损伤和修复,通常在几年甚至几十年内,形成永久性肝脏瘢痕。
Nevertheless, repeated injury and repair, typically over many years and even decades, scars the liver permanently.
瘢痕形成的终末期称为肝硬化,对应于肝脏无法再自我修复的时候。
The end stage of scarring is termed cirrhosis and corresponds to the point where the liver can no longer repair itself.
一旦一个人患有肝硬化,他或她可能会开始出现肝功能不足的迹象。这被称为“失代偿性肝病”。
Once a person has cirrhosis, he or she may begin to show signs of inadequate liver function. This is termed "decompensated liver disease."
虽然药物可以减轻肝衰竭引起的症状,但肝移植是唯一的永久性治愈方法。
Although medications can decrease the symptoms caused by the liver failure, liver transplantation represents the only permanent cure.
失代偿性肝病的体征和症状
Signs and Symptoms of Decompensated Liver Disease
消化道出血:随着肝脏瘢痕越来越多,对门静脉血流的阻力增加,导致门静脉系统的压力增加。
Gastrointestinal bleeding: As the liver becomes increasingly scarred, the resistance to portal blood flow increases leading to increased pressure in the portal venous system.
这种门静脉高压需要血液返回心脏的替代途径。整个腹部的小静脉,但除了肝脏之外,由于在压力增加的情况经它们的血液量异常高,因此变得肿大和薄壁。
This portal hypertension necessitates alternative routes for blood to return to the heart. Small veins throughout the abdomen, but outside of the liver, then become enlarged and thin-walled due to the abnormally high amount of blood flowing through them under increased pressure.
这些脆弱的静脉,称为静脉曲张,通常排列在消化道的某些部分,特别是食道和胃部,并且有破裂和出血的倾向。当出血发生在肠道中时,可能会危及生命。
These fragile veins, called varices, often line portions of the gastrointestinal tract, especially the esophagus and the stomach, and are prone to rupture and bleeding. When bleeding occurs into the intestinal tract, it can be life-threatening.
液体潴留:肝脏的一个功能是合成血液中循环的许多蛋白质,包括白蛋白。
Fluid retention: One function of the liver is to synthesize many of the proteins circulating in the bloodstream, including albumin.
血流中的白蛋白和其他蛋白质通过施加所谓的膨胀(或渗透)压力来保留血管空间中的液体。在肝功能衰竭中,低白蛋白水平迫使液体排出血液,而不能被重新吸收。
Albumin and other proteins in the blood stream retain fluid in the vascular space by exerting what is known as an oncotic (or osmotic) pressure. In liver failure, low albumin levels force fluid out of the bloodstream, which cannot be re-absorbed.
因此,液体积聚在组织和体腔中,最常见的是腹腔,称为“腹水”。液体也可能积聚在腿部(周边或足部水肿)或胸腔(胸腔积水)。
Fluid therefore accumulates in tissues and body cavities, most commonly, in the abdominal cavity, which is termed "ascites." Fluid can also accumulate in the legs (peripheral or pedal edema), or in the chest cavity (hydrothorax).
液体潴留首先通过严格限制膳食盐摄入量来治疗,其次是药物(利尿剂),迫使盐和水通过肾脏流失增加,最后通过针头插入腹部或胸腔进行间歇性引流。
Fluid retention is treated first by strict limitation of dietary salt intake, second with medications (diuretics) that force increased salt and water loss through the kidneys and, lastly, by intermittent drainage through insertion of a needle into the abdominal or chest cavity.
脑病:肝脏无法清除血液中的氨和其他毒素,使这些物质积聚。这些毒素导致认知功能障碍,从睡眠 - 觉醒周期模式紊乱到轻度意识模糊再到昏迷。
Encephalopathy: Failure of the liver to clear ammonia and other toxins from the blood allows these substances to accumulate. These toxins result in cognitive dysfunction that ranges from disturbed sleep-wake cycle patterns to mild confusion to coma.
黄疸:肝脏的主要功能之一是消除血红蛋白的降解产物,血红蛋白是血液中携带氧气的分子。
Jaundice: One of the main functions of the liver is to eliminate the degradation products of hemoglobin, the molecule that carries oxygen in our blood.
胆红素是由肝脏处理和排泄的降解产物之一。在肝功能衰竭时,胆红素不会从体内清除,血液中的胆红素水平升高。然后,皮肤和身体的所有组织将呈现黄色。
Bilirubin is one of those degradation products processed and excreted by the liver. In liver failure, bilirubin is not cleared from the body and bilirubin levels increase in the blood. The skin and all tissues of the body will then assume a yellow color.
慢性肝损伤的原因
Causes of Chronic Liver Injury
病毒性肝炎
Viral Hepatitis
乙型肝炎:乙型肝炎感染占美国所有肝移植的5%,但在世界其他地区,特别是亚洲和澳大利亚/新西兰,肝移植占更大比例。
Hepatitis B: Hepatitis B infection accounts for 5% of all liver transplants performed in the United States but accounts for a larger proportion of liver transplants in other parts of the world, especially Asia and Australia / New Zealand.
丙型肝炎:这是美国肝移植最常见的适应症,影响近50%的肝移植受者。
Hepatitis C: This is the most common indication for liver transplantation in the United States, affecting nearly 50% of all liver transplant recipients.
酒精性肝病
Alcoholic Liver Disease
酗酒引起的肝功能衰竭是美国肝移植的第二大常见指征。大多数中心要求至少六个月的禁欲期,通常是在公认的药物滥用计划(如匿名戒酒会)内,作为移植清单的条件。
Liver failure due to alcohol abuse is the second most common indication for liver transplantation in the United States. Most centers require at least a six-month period of abstinence, often within a recognized substance abuse program such as Alcoholics Anonymous, as a condition of listing for transplantation.
代谢性肝病
Metabolic Liver Disease
非酒精性脂肪性肝炎(NASH):脂肪在肝细胞内的沉积可能导致炎症,从而伤害肝脏留下瘢痕。脂肪肝和NASH发展的危险因素包括肥胖和代谢疾病,如糖尿病和高脂血症(胆固醇升高)。从2000年到2005年,因这种疾病而移植的患者比例增加了35倍。
Non-alcoholic steatohepatitis (NASH): Deposition of fat within liver cells may result in inflammation that injures and scars the liver. Risk factors for the development of fatty liver and NASH include obesity and metabolic conditions such as diabetes and hyperlipidemia (increased cholesterol). The percentage of patients being transplanted for this condition has increased 35 fold from 2000 to 2005.
自身免疫性肝病
Autoimmune Liver Disease
自身免疫性肝炎(患者自身免疫系统对肝脏的破坏)
Autoimmune hepatitis (destruction of the liver by the patient's own immune system)
胆汁淤积性肝病
Cholestatic Liver Diseases
原发性胆汁性肝硬化(PBC)(肝脏内小胆管的破坏)
Primary Biliary Cirrhosis (PBC) (destruction of small bile ducts within the liver)
原发性硬化性胆管炎(PSC)(肝脏内外胆管的破坏)。百分之七十的PSC患者还患有溃疡性结肠炎,这是一种结肠自身免疫性疾病。
Primary Sclerosing Cholangitis (PSC) (destruction of bile ducts inside and outside the liver). Seventy percent of patients with PSC also suffer from ulcerative colitis, an autoimmune disorder of the colon.
新生儿硬化性胆管炎(婴儿肝脏胆管感染和瘢痕形成)
Neonatal sclerosing cholangitis (infection and scarring of the bile ducts in the liver of an infant)
胆道闭锁(肝外无胆管)
Biliary atresia (absence of bile ducts outside the liver)
卡罗利病(肝脏内胆管异常)
Caroli's disease (abnormality of the bile ducts within the liver)
TPN 诱导的胆汁淤积。接受静脉营养(称为全胃肠外营养 (TPN))的患者有时会出现胆汁淤滞(胆汁流动减慢或停止),随着时间的推移,可导致肝损伤和衰竭。
TPN-induced cholestasis. Patients who receive intravenous nutrition, termed total parenteral nutrition (TPN) sometimes develop bile stasis (slowing or stopping of normal bile flow) that can, over time, lead to liver injury and failure.
遗传性肝病
血色病:肝脏中过量的铁沉积
威尔逊氏病:铜代谢异常
α-1抗胰蛋白酶缺乏症:缺乏限制胰蛋白酶活性的基因产物,胰蛋白酶是一种消化蛋白质的酶。随着时间的推移,这会导致肝脏和肺部的进行性破坏。
糖原贮积病(I 型、III 型、IV 型):一种遗传性代谢紊乱
酪氨酸血症:酪氨酸代谢紊乱
血管性肝病
Budd-Chiari综合征是肝静脉的血栓形成(凝血),导致肝脏血流不良。
肝癌
Hepatocellular Carcinoma
肝细胞癌(HCC)是肝脏的原发性癌症,这意味着它起源于异常的肝细胞。肝细胞癌很少发生在正常的非肝硬化肝脏中。然而,在肝硬化的背景下发病率显着增加,特别是导致肝硬化的某些类型的肝脏疾病(乙型肝炎和丙型肝炎,血色病和酪氨酸血症)。
Hepatocellular carcinoma (HCC) is a primary cancer of the liver, meaning that it originates from abnormal liver cells. HCC occurs only rarely in a normal, non-cirrhotic liver. Its incidence is, however, strikingly increased in the background of cirrhosis and, in particular, by certain types of liver disease that lead to cirrhosis (hepatitis B and C, hemachromatosis, and tyrosinemia).
虽然癌症首先在肝脏内开始,但随着它的生长,它可以扩散到其他器官,这个过程称为转移。肝细胞癌最常扩散到肺部或骨骼。扩散到肝脏外的风险随着恶性肿瘤的大小而增加。
Although the cancer first starts within the liver, as it grows it can spread to other organs, a process called metastasis. HCC most frequently spreads to the lungs or to bones. The risk of spread outside of the liver increases with the size of the cancer.
肝移植可以明确治愈肝细胞癌患者,前提是肿瘤尚未扩散到肝脏之外。由于需要肝移植的人数远远多于可用器官的数量,因此已经建立了称为米兰标准的具体指南,以确定哪些HCC患者有资格进行移植。这些标准定义了肿瘤数量和大小的限制,以确保癌症扩散到肝脏外的可能性非常低。
Liver transplantation definitively cures a patient of HCC, provided that the tumor has not spread beyond the liver. Because there are far more people in need of liver transplants than there are available organs, specific guidelines, called the Milan Criteria, have been established to define which patients with HCC are eligible for transplantation. These criteria define limits of tumor number and size that ensure a very low likelihood of cancer spread outside of the liver.
谁不是肝移植的候选人
有许多人患有肝硬化和失代偿性肝病,但并非所有人都是肝移植的合适人选。患者必须能够在手术和潜在的术后并发症中幸存下来,可靠地服用预防排斥和机会性感染的药物,遵守频繁的诊所就诊和实验室检查,并且不从事会伤害肝脏的活动,例如饮酒。下面列出的条件通常被认为是肝移植的绝对禁忌症。
There are many people with cirrhosis and decompensated liver disease but not all are appropriate candidates for liver transplantation. A patient must be able to survive the operation and the potential post-operative complications, reliably take the medications that prevent rejection and opportunistic infections, comply with frequent clinic visits and laboratory tests, and not engage in activity that would injure the liver, such as drinking alcohol. The conditions listed below are generally considered to be absolute contra-indications to liver transplantation.
严重限制短期预期寿命、不可逆的躯体疾病
重度肺动脉高压(平均肺动脉压大于50mmHg)
已扩散到肝脏外的癌症
全身性或无法控制的感染
活性物质滥用(药物和/或酒精)
药物滥用(药物和/或酒精)的不可接受风险
不依从或无法坚持严格的医疗方案的病史
严重、不受控制的精神疾病
肝脏分配
Liver Allocation
分配政策确定任何现有机构将如何分配给候补名单上的许多候选人。在过去的五年中,等待肝移植的患者数量基本保持不变。
我们目前的分配政策以卫生与公众服务部于2000年3月发布的《最终规则》所概述的原则为指导。该规则规定,分配政策应首先考虑受者需要移植的紧迫性。这被称为“最恶心的第一”的概念。
Allocation policy determines how any available organs will be distributed among the many candidates on the waiting list. Over the past five years, the number of patients awaiting a liver transplant has been largely unchanged.
Our current allocation policy is guided by the principles outlined by the Final Rule, issued by the Department of Health and Human Services in March 2000. The Rule stipulates that allocation policy should give primary consideration to the urgency of a recipient's need for transplantation. This has come to be known as the concept of "sickest first."
梅尔德得分
MELD Score
已经进行了大量的研究,试图了解如何准确地确定一个人由肝病引起的患病严重程度。一种称为MELD(终末期肝病模型)的评分系统已被确定为高度预测慢性肝病引起的死亡风险。
Much research has gone into trying to understand how to accurately determine how sick a person is from his or her liver disease. A scoring system, called MELD (Model for End-stage Liver Disease), has been identified as highly predictive of the risk of death posed by chronic liver disease.
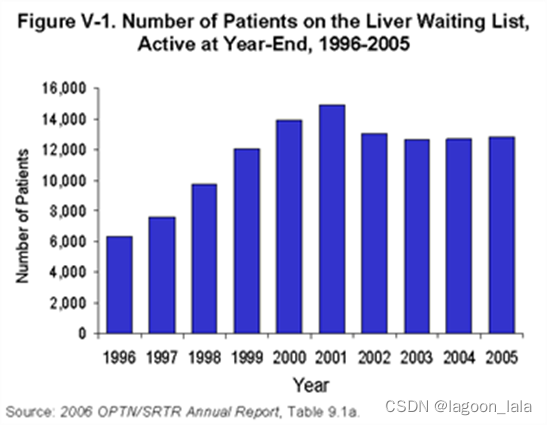
(候补名单图)
MELD评分由三个客观且现成的实验室检查结果决定:
The MELD score is determined by the results of three objective and readily available laboratory tests:
1.总胆红素,即黄疸的量度
1.Total bilirubin, a measure of jaundice
2.凝血酶原时间,即凝血能力的量度
Prothrombin time, a measure of clotting ability
3.肌酐,即肾功能的量度
3.Creatinine, a measure of kidney function.
将这三个数字输入到以下公式中可得到实际的数字分数。
Inputting these three numbers into the following formula yields the actual numerical score.
MELD = 3.8 X log e(total bilirubin [mg/dL]) + 11.2 X log e(INR) + 9.6 X log e(creatinine [mg/dL])
A MELD calculator is used to determine MELD scores.
随着患者肝功能恶化,实验室检查结果增加,他/她的MELD分数也会增加,这将使患者在候补名单上处于更高的位置。因此,MELD评分最高的患者(病情最严重的患者)位于列表的顶部。然而,列表是按血型组织的。当供体肝脏可用时,将确定供体的血型,并为该血型列表顶部的人提供器官。如果这个人病得太重或由于某种原因不接受肝脏,那么肝脏就会被提供给名单上的下一个人,依此类推,直到找到合适的接受者。
As a patient's liver function deteriorates, the laboratory test results increase as will his/her MELD score which will move the patient to a higher position on the waitlist. The patient with the highest MELD score (the sickest patient) is therefore at the top of the list. Lists are, however, organized by blood type. When a donor liver becomes available, the blood type of the donor is determined and the person at the top of the list for that blood group is offered the organ. If that person is too sick or does not accept the liver for whatever reason, the liver is then offered to the next person on the list and so forth until a suitable recipient is found.
地理和DSAs
肝脏分配政策的另一个复杂因素是地理。美国分为11个区域,每个区域又分为多个捐助服务区。
美国的11个多捐助方服务区(DSA)
DSA是器官分配的最小或“本地”单位。大多数情况下,在特定DSA中从捐赠者处获得的器官被分配到同一DSA内的候选接受者。这项政策的出现是一种尽量减少器官运输和保存时间的方法。然而,最终规则强调了疾病严重程度的重要性,并低估了地理因素对器官分配政策的影响。因此,如果有肝病敏锐度和严重程度最高的候选人 - 那些由于急性/暴发性肝功能衰竭或原发性无功能而被列为“状态1”的候选人 - 肝脏按区域或国家分配。
The DSAs are the smallest or the "local" unit of organ allocation. Most frequently, organs that are procured from donors in a specific DSA are allocated to candidate recipients within the same DSA. This policy arose as an approach to minimize times for organ transportation and preservation. The Final Rule, however, emphasized the importance of disease severity and discounted the impact of geography in organ allocation policy. Therefore, if there are candidates with the highest acuity and severity of liver disease - those listed as "Status 1" because of acute / fulminant hepatic failure or primary non-function - livers are allocated on a regional or national basis.
器官捐献者的类型
脑死亡器官捐献者
Brain dead organ donors
大多数用于移植的肝脏是从脑死亡患者那里获得的。
Most livers used for transplantation are obtained from patients that are brain dead.
脑死亡通常是由于钝性损伤(例如,机动车辆或摩托车事故对头部的撞击)或穿透伤(例如,枪伤)对头部造成的大中风或头部的巨大创伤。创伤已经停止了所有的大脑功能,尽管包括肝脏在内的其他器官可能继续正常运作。
Brain death is usually due to a large stroke or massive trauma to the head from blunt injury (for example, impact to the head from a motor vehicle or a motorcycle accident) or penetrating injury (for example, a gun shot wound). The trauma has stopped all brain function although other organs including the liver may continue to function normally.
脑死亡有严格的定义, 即完全没有任何类型的脑功能。因为符合脑死亡标准的患者在法律上已经死亡,所以他们是适当的器官和组织供体。在美国,脑死亡者的家人必须同意器官和/或组织捐赠。在其他国家,如法国,除非家人反对,否则推定并允许同意器官捐献。
There are strict definitions as to what constitutes brain death based on the complete absence of any type of brain function. Because patients that meet criteria for brain death are legally dead, they are appropriate organ and tissue donors. In the United States, the family of someone who is brain dead must provide consent for organ and/or tissue donation. In other countries, such as France, consent for organ donation is presumed and allowed, unless the family objects.
通常,移植中心的患者将从特定供体接收器官,他们将派遣一组外科医生来采购相关器官。器官获取程序在捐赠者医院的手术室进行。器官被移除和保存,以优化其在储存和运输期间的状况。然后将每个采购的器官运送到指定的接受者的医院等待。
Typically, transplant centers whose patients will be receiving organs from a particular donor will dispatch a team of surgeons to procure the relevant organ. The organ procurement procedure takes place in an operating room in the donor's hospital. Organs are removed and preserved in a fashion to optimize their condition during the storage and transportation time period. Each procured organ is then transported to the hospitals where the designated recipient awaits.
心源性死亡器官捐献者
Cardiac death organ donors
有时,患者遭受毁灭性的脑损伤,并带有令人沮丧的神经预后,但不符合定义脑死亡的严格标准,因为仍有可检测到的脑功能。在这些情况下,患者家属可能会决定撤回维持生命的医疗支持,目的是让患者死亡。在这种情况下,死亡不是由脑死亡定义的,而是由心源性死亡定义的。器官捐献可以在心脏死亡后发生,但同样,只有在家人同意的情况下。
Sometimes a patient suffers a devastating brain injury and carries a dismal neurological prognosis but fails to meet the strict criteria defining brain death in that there is still detectible brain function. In these circumstances, the patient's family may decide to withdraw life-sustaining medical support with the intention of allowing the patient to die. In this scenario, death is not defined by brain death but rather cardiac death. Organ donation can occur after cardiac death but, again, only if the family gives consent.
只有在家属决定撤回支持后,患者才被考虑进行死后器官捐献。在这种情况下,根据家庭的意愿,由患者的医生管理,支持被撤回,并且允许患者自主呼吸(撤掉呼吸机)。患者的医生,不参与器官移植任何方面的人,在场以确定心脏何时停止跳动和循环停止,使患者不再有任何生命迹象。然后他或她宣布病人死亡。
Only AFTER the family's decision to withdraw support may the patient be considered for organ donation after death. Under these circumstances, support is withdrawn, as desired by the family and managed by the patient's physician, and the patient is allowed to expire. The patient's physician, someone who is not involved in any aspect of organ transplantation, is present to determine when the heart stops beating and circulation has stopped such that the patient no longer has any signs of life. He or she then declares the patient's death.
然后进行紧急手术以保存和切除用于移植的器官。与脑死亡相比,这种心源性死亡模式在两个时间段内导致器官损伤增加。
An urgent operation is then performed to preserve and remove organs for transplantation. This mode of cardiac death, in contrast to brain death, results in increased injury to the organs during two time periods.
第一个时期是生命支持退出和死亡之间的时期。随着供体的呼吸和循环恶化,器官可能不再接受足够的氧气。
The first period is that between withdrawal of life support and death. As the donor's breathing and circulation deteriorates, the organs may no longer be receiving sufficient oxygen.
第二个时间段构成为死亡后的几分钟,直到用保存液冲洗器官并冷冻。因此,从心脏死亡供体处获得的肝脏与原发性无功能或早期器官功能差、肝动脉血栓形成和胆道并发症的风险增加有关(见并发症部分)。
The second time period constitutes the minutes immediately after death and until the organs are flushed with preservation solution and cooled. As a result, livers procured from cardiac death donors are associated with an increased risk of primary non function or poor early organ function, hepatic artery thrombosis, and biliary complications (see Complications section).
活体捐赠者
Living Donors
虽然每个人都只有一个肝脏,如果没有它,就会死去,但有可能将一部分肝脏捐献给另一个人进行移植。节段解剖学(见下图)允许外科医生根据接受者对肝脏组织的要求创建不同大小的移植物。供体和受体的部分肝脏都会生长,为两个人提供正常的肝功能。
Although each person has only one liver and would die without it, it is possible to donate a portion of the liver for transplantation into another individual. The segmental anatomy (see figure below) allows surgeons to create grafts of varying size, depending upon the recipient's requirement for liver tissue. The partial livers in both the donor and the recipient will grow to provide normal liver function for both individuals.
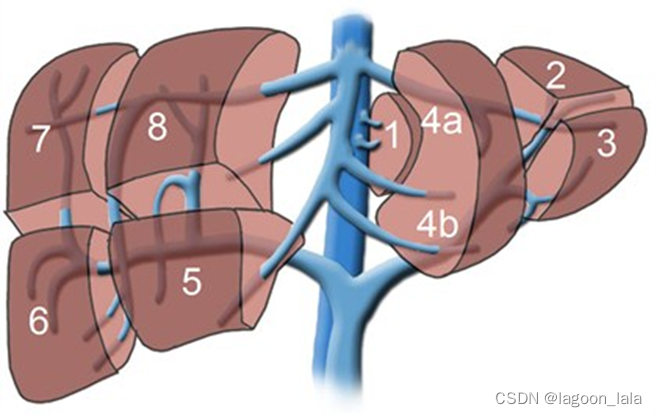
(图: 肝脏分为八个部分(segments),反映了门静脉和胆管的八个主要区域(divisions)。
http://www.healcentral.org/)
从历史上看,该程序是为了能够移植儿童而开发的,因为很难从已故的供体中找到适合该组的肝脏。为了移植儿童,通常使用由第2段和第3段组成的移植物,称为左侧段,代表整个肝脏体积的20-25%。
Historically, this procedure was developed to enable transplantation of children as it was difficult to find suitable livers from deceased donors for this group. To transplant a child, typically a graft comprised of segments 2 and 3, together known as the left lateral segment representing 20-25% of the whole liver volume, is used.
然而,移植年龄较大的儿童或体型小的成年人可能需要第2,3和4段,一起称为左叶,约占整个肝脏体积的40%。然而,在过去十年中,该技术已进一步扩展,以允许使用右叶,节段5,6,7和8移植成人,约占总肝容量的60%。成人到成人活体供体肝移植是高度复杂且技术上具有挑战性的过程,对供体和受体都具有重大风险。
Transplantation of an older child or perhaps a petite adult, however, may require segments 2, 3, and 4, together known as the left lobe and representing approximately 40% of the whole liver volume. During the past decade, however, this technique has been further extended to enable transplantation of adults using the right lobe, segments 5, 6, 7, and 8, which account for approximately 60% of the total liver volume. An adult-to-adult living donor liver transplant is highly complex and technically challenging procedure that carries a significant risk for both the donor and the recipient.
肝移植手术
The Liver Transplant Operation
肝脏移植涉及切除和准备供体肝脏,切除患病肝脏以及植入新器官。
A liver transplant involves the removal of and preparation of the donor liver, removal of the diseased liver, and implantation of the new organ.
肝脏有几个关键连接,必须重新建立新器官才能接收血流并从肝脏排出胆汁。必须重新连接的结构是下腔静脉、门静脉、肝动脉和胆管。连接这些结构的确切方法取决于特定的供体和解剖学或受体解剖问题,在某些情况下,还取决于受体疾病。
The liver has several key connections that must be re-established for the new organ to receive blood flow and to drain bile from the liver. The structures that must be reconnected are the inferior vena cava, the portal vein, the hepatic artery, and the bile duct. The exact method of connecting these structures varies depending on specific donor and anatomy or recipient anatomic issues and, in some cases, the recipient disease.
对于接受肝移植的人,手术室中的事件顺序如下:
For someone undergoing liver transplantation, the sequence of events in the operating room is as follows:
1.切口
2.评估腹部是否有异常导致无法进行肝移植(例如:未确诊的感染或恶性肿瘤)
3.切除原肝脏(解剖附着在腹腔的肝脏)
4.隔离重要结构(肝脏上方、后面和下方的下腔静脉;门静脉;胆总管;肝动脉)
5.切断上述结构和去除原患病的肝脏。(图7没找到)
6.缝合新肝脏:首先,通过连接供体和接受者的下腔静脉和门静脉来重新建立静脉血流。接下来,通过缝合供体和受体的肝动脉来重新建立动脉血流。最后,通过缝合供体和受体的胆总管来实现胆道引流。
7.确保充分控制出血
8.切口闭合
1.Incision
2.Evaluation of the abdomen for abnormalities that would preclude liver transplantation (for example: undiagnosed infection or malignancy)
3.Mobilization of the native liver (dissection of the liver attachments to the abdominal cavity)
4.Isolation of important structures (the inferior vena cava above, behind, and below the liver; the portal vein; the common bile duct; the hepatic artery)
5.Transection of the above mentioned structures and removal of the native, diseased liver. (Figure 7)
6.Sewing in the new liver: First, venous blood flow is re-established by connecting the donor's and the recipient's inferior vena cava and portal veins. Next, arterial flow is re-established by sewing the donor's and recipient's hepatic arteries. Finally, biliary drainage is achieved by sewing the donor's and recipient's common bile ducts.
7.Ensuring adequate control of bleeding
8.Closure of the incision
手术并发症
Surgical Complications
与任何外科手术一样,除了任何住院患者可能发生的许多可能的并发症外,还可能发生与手术相关的并发症。肝移植可能遇到的一些特定问题包括:
As with any surgical procedure, complications related to the operation may occur, in addition to the many possible complications that may happen to any patient who is hospitalized. Some of the problems specific to liver transplantation that may be encountered include:
新移植肝脏的原发性无功能或功能差发生在大约1-5%的新移植中。如果肝功能不能充分或足够快地改善,患者可能迫切需要第二次移植才能存活。
Primary non-function or poor function of the newly transplanted liver occurs in approximately 1-5% of new transplants. If the function of the liver does not improve sufficiently or quickly enough, the patient may urgently require a second transplant to survive.
1.肝动脉血栓形成或肝动脉凝固(将含氧血液从心脏输送到肝脏的血管)发生在所有已故供体移植的2-5%中。在接受活体供体移植的患者中,风险加倍。肝细胞本身通常不会因肝动脉的血流损失而受到影响,因为它们主要由门静脉血流供血滋养。相反,胆管强烈依赖肝动脉的营养,血流失可能导致胆管瘢痕形成和感染。如果发生这种情况,则可能需要进行另一次移植。
Hepatic artery thrombosis, or clotting of the hepatic artery (the blood vessel that brings oxygenated blood from the heart to the liver) occurs in 2-5% of all deceased donor transplants. The risk is doubled in patients who receive a living donor transplant. The liver cells themselves typically do not suffer from losing blood flow from the hepatic artery because they are primarily nourished by blood by the portal blood flow. In contrast, the bile ducts depend strongly on the hepatic artery for nutrition and loss of that blood flow may lead to bile duct scarring and infection. If this occurs, then another transplant may be necessary.
2.门静脉血栓形成或大静脉凝固,将血液从腹部器官(肠,胰腺和脾脏 - 属于门静脉循环的器官)带到肝脏很少发生。这种并发症可能需要也可能不需要第二次肝移植。
Portal vein thrombosis or clotting of the large vein that brings blood from the abdominal organs (the intestines, the pancreas, and the spleen - the organs that belong to the portal circulation) to the liver occurs infrequently. This complication may or may not require a second liver transplant.
3.胆道并发症:一般来说,有两种类型的胆道问题:渗漏或狭窄。胆道并发症影响约15%的已故供体移植和高达40%的活体供体移植。
Biliary complications: In general, there are two types of biliary problems: leak or stricture. Biliary complications affect approximately 15% of all deceased donor transplants and up to 40% of all living donor transplants.
(1)胆道渗漏是指胆汁从胆管渗出并进入腹腔。最常见的是,这发生在供体和受体胆管缝合在一起的地方。这通常通过将支架或塑料管穿过胃和小肠的连接,然后允许连接愈合来治疗。在活体供体或分裂肝脏移植的情况下,胆汁也可以从肝脏的切口边缘泄漏。通常,在移植手术过程中,沿着切口边缘放置引流管,以去除可能泄漏的任何胆汁。只要胆汁不聚集在腹部,患者就不会生病。泄漏通常会随着时间的推移而愈合,但可能需要额外的治疗程序。
Biliary leak means that bile is leaking out of the bile duct and into the abdominal cavity. Most frequently, this occurs where the donor and recipient bile ducts were sewn together. This is often treated by placing a stent, or plastic tube, across the connection through the stomach and small intestine and then allowing the connection to heal. In the case of living donor or split liver transplants, bile can also leak from the cut edge of the liver. Typically, a drain is placed and left during the transplant operation along the cut edge to remove any bile that may leak. As long as the bile does not collect in the abdomen, the patient does not become ill. Leaks will often heal with time, but may require additional treatment procedures.
(2)胆道狭窄意味着胆管变窄,导致胆汁流动相对或完全阻塞并可能感染。最常见的是,狭窄发生在单个部位,再次将供体和受体导管缝合在一起。这种狭窄通常可以通过用球囊扩张狭窄的区域和/或在狭窄处插入支架来治疗。如果这些方法不成功,通常进行手术以在肝脏胆管和肠段之间建立新的连接。极少数情况下,胆道狭窄发生在整个胆道树的多个或无数个部位。这种情况最常发生的原因是在肝脏不在供体或受体循环中期间,胆道树保存得很差。从心脏死亡供体获得的肝脏比从脑死亡供体获得的肝脏风险更高。或者,如果胆道树由于肝动脉异常导致血液供应不足,则可能发生弥漫性胆道狭窄。
Biliary stricture means narrowing of the bile duct, resulting in relative or complete blockage of the bile flow and possible infection. Most frequently, the narrowing occurs at a single site, again where the donor and recipient ducts are sewn together. This narrowing can often be treated by dilating the narrowed area with a balloon and/or inserting a stent across the stricture. If these methods are unsuccessful, surgery is often done to create a new connection between the liver's bile duct and a segment of intestine. Rarely, biliary strictures occur at multiple or innumerable sites throughout the biliary tree. This occurs most frequently because the biliary tree was poorly preserved during the period when the liver was not in either the donor or recipient circulation. Livers procured from cardiac death donors are at higher risk than those from brain dead donors. Alternatively, diffuse biliary strictures may occur if the biliary tree has inadequate blood supply because of an abnormality with the hepatic artery.
4.出血是任何外科手术的风险,但由于手术的面积大以及凝血需要肝脏产生的因子,肝移植后的特殊风险。大多数移植患者出血量很小,手术后可能会再输血。如果出血量大或出血过快,通常需要返回手术室控制出血。一般来说,大约10%的移植受者需要第二次手术来止血。
Bleeding is a risk of any surgical procedure but a particular risk after liver transplantation because of the extensive nature of the surgery and because clotting requires factors made by the liver. Most transplant patients bleed a minor amount and may get additional transfusions after the operation. If bleeding is substantial or brisk, return to the operating room for control of bleeding is often necessary. In general, approximately 10% of transplant recipients will require a second operation for bleeding.
5.感染 - 感染可能发生在任何手术产生的伤口愈合过程中。肝移植受者也有腹部深处感染的风险,特别是如果有血液或胆汁(来自胆汁泄漏)的聚集。免疫抑制药物以及肝功能衰竭病史会增加肝移植受者在移植后发生感染的风险。
Infection - Infections can occur during the healing of the wound created by any operation. Liver transplant recipients are also at risk for infections deep within the abdomen, particularly if there is a collection of blood or bile (from a bile leak). The immunosuppressive medications along with the history of liver failure increase the liver transplant recipient's risk for developing an infection after transplantation.
免疫抑制
Immunosuppression
人体已经发展出一系列针对细菌,病毒和肿瘤的非常复杂的防御措施。免疫系统的机器已经进化了数百万年,以识别和攻击任何外来的或非“自我”的东西。不幸的是,移植器官属于外来的范畴,而不是自我。许多药物被给予移植受者,以抑制其免疫系统的反应,以保持器官的安全和免受免疫攻击。如果免疫系统没有被充分削弱,那么排斥反应 - 免疫系统识别,攻击和伤害移植器官的过程 - 随之而来。
下面列出了通过抑制免疫系统来防止排斥的常用药物。它们通过不同的机制来削弱免疫系统对刺激的反应,并与不同的副作用相关。因此,这些药物经常以各种组合使用,以增加整体免疫抑制作用,同时最大限度地减少副作用。
1.皮质类固醇(静脉注射甲基泼尼松龙;泼尼松龙口服):皮质类固醇是一类抗炎剂,可抑制细胞因子的产生,细胞因子是由免疫系统细胞产生的信号分子,用于协调和增强免疫反应。因此,皮质类固醇可防止淋巴细胞的活化,淋巴细胞是针对移植器官的免疫反应的主要士兵。这被认为可以以非特异性方式阻止T细胞(淋巴细胞的一个亚群)活化。皮质类固醇的副作用广泛,包括高血糖、高血压、骨密度下降和伤口愈合受损,
2.钙调磷酸酶抑制剂(环孢素,他克莫司):这类药物阻断钙调磷酸酶的功能,钙调磷酸酶是一种非常重要的淋巴细胞信号通路的关键分子,可触发多种细胞因子的产生。这些药物大约在20年前首次开发,彻底改变了器官移植。它们大大降低了排斥的发生率,延长了移植器官的寿命,从而开创了移植和免疫抑制的当代时代。不幸的是,这些药物具有显着的副作用。最严重的毒性,特别是长期使用,是肾损伤。钙调磷酸酶抑制剂也会升高血压、葡萄糖水平和胆固醇,并引起震颤和头痛。
3.霉酚酸酯(Cellcept®,Myfortic®):这种药物在体内转化为霉酚酸,其抑制淋巴细胞复制DNA的能力,DNA是每个细胞所必需的遗传物质。如果淋巴细胞不能合成DNA,那么它们就无法分裂以产生额外的细胞。因此,吗替麦考酚酯通过防止淋巴细胞的增殖来抑制免疫反应。吗替麦考酚酯的主要副作用会影响肠道系统,导致胃部不适和/或腹泻。它还可以抑制骨髓功能,从而降低白细胞(抗感染细胞),红细胞(携氧细胞)和血小板(凝血剂)的血液水平。
4.mTOR抑制剂(西罗莫司;依维莫司):mTOR代表哺乳动物雷帕霉素的靶标。mTOR属于称为激酶的酶家族,参与细胞周期的检查点调节,DNA修复和细胞死亡。mTOR的抑制阻止T细胞通过细胞周期的各个阶段,导致细胞周期停滞。因此,淋巴细胞不能分裂以放大免疫反应。mTOR抑制剂的副作用包括骨髓抑制,伤口愈合不良和胆固醇水平升高。
5.靶向IL-2受体的抗体,IL-2受体是一种放大免疫反应的信号分子(巴利昔单抗,达克珠单抗):T细胞,急性排斥的因子,在受到刺激时表达越来越多的IL2受体。IL-2受体允许免疫反应的持续扩增。因此,这种受体的阻断会抑制免疫反应。这些抗体最常在移植时开始的短时间内使用,以在排斥风险最高的时期提供额外的免疫抑制。立即的副作用包括发热、皮疹、细胞因子释放综合征和过敏反应。它们似乎确实增加了与其他免疫抑制药物联合使用的感染风险。
6.从循环中去除T细胞的抗体(胸腺球蛋白®,OKT-3®):这些药物是靶向免疫系统不同细胞,结合它们,灭活和去除它们的分子。它们可以在肝移植时使用。但更常见的是用于治疗严重排斥反应或对较差治疗策略无反应的排斥反应。这些药物的直接副作用包括发烧和皮疹到细胞因子释放综合征,导致闪电肺水肿和低血压。这些药物也可能导致PTLD和皮肤癌的发病率增加(见下文)
7.研究药物 - 随着我们对免疫系统的了解的提高,研究人员已经确定了在身体对移植器官的反应中起作用的新细胞,分子和途径。每一项发现都以药物开发的新靶点的形式提供了新的机会。其中一些药物目前正在临床试验中进行测试,以确定它们是否安全有效地用于移植。未来几代药物有望在预防排斥反应方面更具特异性,而不会显着干扰免疫系统的其他功能或引起非免疫副作用。
The human body has developed a very sophisticated series of defenses against bacteria, viruses, and tumors. The machinery of the immune system has evolved over millions of years to identify and attack anything that is foreign or not "self." Unfortunately, transplanted organs fall into the category of foreign, not self. A number of drugs are given to transplant recipients to dampen the responses of their immune system in an attempt to keep the organ safe and free of immunologic attack. If the immune system is not sufficiently weakened, then rejection - the process by which the immune system identifies, attacks, and injures the transplanted organ - ensues.
Commonly used drugs to prevent rejection by suppressing the immune system are listed below. They work through different mechanisms to weaken the immune system's responses to stimuli and are associated with different side effects. As a result, these medications are frequently used in various combinations which increase the overall immunosuppressive effect while minimizing side effects.
Corticosteroids (methylprednisolone is given intravenously; prednisone is given orally): Corticosteroids are a class of anti-inflammatory agents that inhibit production of cytokines, the signaling molecules produced by cells of the immune system to orchestrate and intensify the immune response. Corticosteroids therefore prevent activation of lymphocytes, the main soldiers of the immune response against transplanted organs. This is thought to prevent T-cell (a subset of lymphocytes) activation in a non-specific manner. Side effects of corticosteroids are broad and include hyperglycemia, hypertension, decreased bone density, and impaired wound healing,
Calcineurin inhibitors (cyclosporine, tacrolimus): This class of drugs blocks the function of calcineurin, a molecule critical to a very important lymphocyte signaling pathway that triggers the production of multiple cytokines. These drugs, first developed approximately 20 years ago, revolutionized organ transplantation. They substantially reduced the incidence of rejection, improved the longevity of transplanted organs and thereby ushered in the contemporary era of transplantation and immunosuppression. Unfortunately, these drugs come with a significant side effect profile. The most serious toxicity, particularly with long-term use, is kidney injury. Calcineurin inhibitors also raise blood pressure, glucose levels, and cholesterol - and cause tremors and headaches.
Mycophenolate mofetil (Cellcept®, Myfortic®): This drug is converted in the body to mycophenolic acid, which inhibits the ability of lymphocytes to replicate DNA, the genetic material essential to every cell. If lymphocytes cannot synthesize DNA, then they are unable to divide to generate additional cells. Mycophenolate mofetil, therefore, dampens the immune response by preventing proliferation of lymphocytes. The primary side effects of mycophenolate mofetil affect the intestinal system resulting in stomach upset and/or diarrhea. It can also depress bone marrow function and thereby, reduce blood levels of white cells (infection fighting cells), red cells (oxygen carrying cells), and platelets (clotting agents).
mTOR inhibitors (sirolimus; everolimus): mTOR stands for mammalian Target Of Rapamycin. mTOR belongs to a family of enzymes known as kinases and is involved in checkpoint regulation of the cell cycle, DNA repair, and cell death. Inhibition of mTOR stops T cells from progressing through the various phases of the cell cycle, leading to cell cycle arrest. Thus, lymphocytes are not able to divide to amplify the immune response. Side effects of mTOR inhibitors include bone marrow depression, poor wound healing, and increased cholesterol levels.
Antibodies that target the IL-2 receptor, a signaling molecule that amplifies the immune response (basiliximab, daclizumab): T cells, the agents of acute rejection, express increasing amounts of IL2-receptors when they are stimulated. The IL-2 receptor allows ongoing amplification of an immune response. Blockage of this receptor therefore dampens the immune response. These antibodies are most frequently used for a short time period beginning at the time of transplant to provide additional immunosuppression during this period of highest rejection risk. Immediate side effects include fever, rash, cytokine release syndrome, and anaphylaxis. They do appear to increase the risk of infections hen combined with other immunosuppressive medications.
Antibodies that remove T cells from the circulation (Thymoglobulin®, OKT-3®): These agents are molecules that target different cells of the immune system, bind them, inactivate, and remove them. They can be used at the time of liver transplantation. but more often are used to treat severe rejection or rejection that does not respond to lesser treatment strategies. Immediate side effects of these medications range from fever and rash to cytokine release syndrome resulting in flash pulmonary edema and hypotension. These drugs may also result in increased incidence of PTLD and skin cancers (see below)
investigational drugs - As our understanding of the immune system improves, researchers have identified new cells, molecules, and pathways that play a role in the body's response to transplanted organs. Each discovery presents new opportunities in the form of new targets for drug development. Some of these medicines are currently being tested in clinical trials to determine if they are safe and effective for use in transplantation. Future generations of drugs will hopefully be more specific in preventing rejection without interfering significantly with the other functions of the immune system or causing non-immunologic side effects.
排斥反应
Rejection
排斥反应是一个术语,适用于由受体对移植器官的免疫系统反应引起的器官功能障碍。肝脏损伤通常由免疫细胞、T 细胞或 T 淋巴细胞介导。排斥通常不会引起任何症状;患者没有任何不同的感觉或注意到任何事情。第一个体征通常是肝脏实验室检查结果异常升高。当怀疑排斥反应时,进行肝活检。肝活检很容易作为床边手术,使用通过皮肤引入的特殊针头。然后在显微镜下分析和检查组织,以确定肝损伤的模式,并寻找免疫细胞的存在。
Rejection is a term that is applied to organ dysfunction caused by the recipient's immune system reaction to the transplanted organ. Injury to the liver is typically mediated by immune cells, T cells or T lymphocytes. Rejection typically causes no symptoms; patients do not feel any differently or notice anything. The first sign is usually abnormally elevated liver laboratory test results. When rejection is suspected, a liver biopsy is performed. Liver biopsies are easily done as a bedside procedure using a special needle that is introduced through the skin. The tissue is then analyzed and inspected under the microscope to determine the pattern of liver injury and also to look for the presence of immune cells.
25-50%的肝移植受者在移植后第一年内发生急性细胞排斥反应,在移植后的前四到六周内风险最高。一旦做出诊断,治疗相当简单,通常非常有效。一线治疗是大剂量皮质类固醇( 见前文免疫抑制小节)。患者的维持免疫抑制方案也升级,以防止随后的排斥反应。一小部分急性排斥发作(约 10-20%)对皮质类固醇治疗无反应,被称为“类固醇难治性”,需要额外治疗。
Acute cellular rejection occurs in 25-50% of all liver transplant recipients within the first year after transplantation with the highest risk period within the first four to six weeks of transplantation. Once the diagnosis is made, treatment is fairly straightforward and generally very effective. The first line of treatment is high dose corticosteroids (see Immunosuppression section). The patient's maintenance immunosuppression regimen is also escalated to prevent subsequent rejection. A small proportion of acute rejection episodes, approximately 10-20%, does not respond to corticosteroid treatment and are termed "steroid refractory," requiring additional treatment.
排斥治疗的第二线是强抗体制剂( 见前文免疫抑制小节)。在肝移植中,与其他器官不同,急性细胞排斥反应通常不会影响移植物存活的总体机会。这被认为是因为肝脏在受伤时具有独特的再生能力,从而恢复完整的肝功能。
The second line of rejection treatment is strong antibody preparations (see Immunosuppression Section). In liver transplantation, unlike other organs, acute cellular rejection does not generally affect overall chances for graft survival. This is believed to be because the liver has the unique ability to regenerate when injured thereby restoring full liver function.
慢性排斥反应发生在所有移植受者中5%或更少。发生慢性排斥反应的最强危险因素是急性排斥反应和/或难治性急性排斥反应的反复发作。肝活检显示胆管丢失和小动脉闭塞。从历史上看,慢性排斥反应很难逆转,通常需要重复肝移植。今天,随着我们大量选择免疫抑制药物,慢性排斥反应通常是可逆的。
Chronic rejection occurs in 5% or less of all transplant recipients. The strongest risk factor for the development of chronic rejection is repeated episodes of acute rejection and/or refractory acute rejection. Liver biopsy shows loss of bile ducts and obliteration of small arteries. Chronic rejection, historically, has been difficult to reverse, often necessitating repeat liver transplantation. Today, with our large selection of immunosuppressive drugs, chronic rejection is more often reversible.
复发性疾病
Recurrent Disease
导致患者自身肝脏衰竭的一些过程会损害新肝脏并最终破坏它。也许最好的例子是乙型肝炎感染。在20世纪90年代初,因乙型肝炎感染接受肝移植的患者五年生存率不到50%。这些患者中绝大多数患有乙型肝炎病毒对新肝脏的非常积极的再感染。然而,在20世纪90年代,移植中心开发并广泛建立了几种预防新肝脏再感染和损伤的药物和策略。这些方法非常成功,因此复发性疾病不再是问题。乙型肝炎曾经被认为是移植的禁忌症,现在与良好的结果相关,优于肝移植的许多其他适应症。
目前,我们复发性疾病的主要问题集中在丙型肝炎上。任何携带血液中循环的丙型肝炎病毒进入移植期的患者在移植后都会有持续的丙型肝炎。然而,那些已经完全清除病毒并且血液中没有可测量的丙型肝炎的人在移植后不会患有丙型肝炎。
与乙型肝炎不同,乙型肝炎的复发性疾病导致肝功能衰竭发生得非常快,复发性丙型肝炎通常会导致肝功能更逐渐丧失。只有一小部分丙型肝炎受者(约5%)在移植后两年内复发肝硬化和终末期肝病。
大多数患者病情逐渐进展,在移植后约 10 年,多达一半的患者会出现肝硬化。干扰素制剂与利巴韦林联合使用,广泛用于移植前丙型肝炎患者,也可以在移植后开处方。永久治愈的机会略低于移植前的治疗。此外,该治疗与副作用的显着补充有关。复发性疾病是导致丙型肝炎肝移植受者与没有丙型肝炎的肝移植受者相比,移植后中期和长期结果较差的原因(图8)。
其他几种疾病也可能在移植后复发,但通常这种疾病是轻微的,只是缓慢进展。原发性硬化性胆管炎(PSC)和原发性胆汁性肝硬化(PBC)在大约10-20%的时间内复发,并且仅在极少数情况下导致复发性肝硬化和终末期肝病。也许当今时代最大的未知数是移植后的脂肪肝疾病,因为它显然是一个频率增加的问题。脂肪肝疾病可能发生在那些移植为NASH的人身上,也可以发生在因其他适应症而移植的患者中,并发展为脂肪肝的危险因素。移植后脂肪肝复发的频率、轨迹和预后及其病程是研究的活跃领域。
机会性感染和癌症
Opportunistic Infections and Cancer
如前所述,免疫系统的主要作用是识别和攻击任何外来或非自我的东西。主要靶标不是移植器官,而是细菌,病毒,真菌和其他引起感染的微生物。采取免疫抑制措施会削弱移植受者对感染的防御能力
因此,移植受者不仅患上可能影响所有人的标准感染,而且“机会性”感染的风险增加,这种感染只发生在免疫系统受损的人身上。免疫系统的变化使移植受者易患不同感染,这取决于相对于其移植操作的时间。
它们可以分为三个时期:第一个月,第一个月到第六个月,以及六个月以上。在第一个月,细菌和真菌感染是最常见的。病毒感染(如巨细胞病毒)和其他异常感染(如肺结核和卡氏肺孢子虫)在前六个月内可见。
除了抵抗感染,免疫系统还可以对抗癌症。据信,健康的免疫系统在异常癌细胞繁殖并生长成肿瘤之前检测并消除它们。众所周知,移植受者患几种特定类型癌症的风险增加。
移植后淋巴调节障碍 (PTLD)
移植后淋巴循环障碍(PTLD)是一种不寻常的癌症类型,仅在移植受者中出现,正如其名称所暗示的那样。它几乎总是与爱泼斯坦 - 巴尔病毒(EBV)有关,EBV是导致传染性单核细胞增多症或“接吻病”的病毒。
大多数成年人接触过EB病毒,最常见于他们的童年或青少年时期。对于这些患者,移植后可发生EBV相关的PTLD,因为免疫抑制允许病毒重新激活。相比之下,许多儿童在没有接触过EBV的情况下进行肝移植。如果患者在移植后暴露于EBV,因此在免疫抑制的影响下,他们可能无法控制感染。
PTLD在EBV感染的B细胞(淋巴细胞的一个亚群)以不受控制的方式生长和分裂时出现在任何一种情况下。由于它基本上是免疫系统受损的结果,因此第一线治疗是简单地停止或大幅减少免疫抑制。虽然这种方法经常有效,但它也有移植物排斥的风险,这将导致免疫抑制增加。最近,一种特异性消除B细胞(EBV感染的细胞)的药物已经问世。
今天,一种常见的方法是将这种药物利妥昔单抗与免疫抑制药物的不那么剧烈的削减相结合。如果这种方法不能控制PTLD,则使用更常规的化疗药物方案来治疗非免疫抑制患者中发生的淋巴瘤。大多数PTLD病例可以通过保存移植器官来成功治疗。
非黑色素瘤皮肤癌
皮肤癌是移植后人群中最常见的恶性肿瘤。接受器官移植的患者的皮肤癌发病率在10岁时为27%,反映出风险相对于正常人群增加了25倍。鉴于这种重大风险,强烈建议所有移植受者尽量减少阳光照射。
此外,应定期检查所有移植受者,以确保任何皮肤癌的早期诊断和快速治疗。有证据表明,西罗莫司是一类mTOR抑制剂中的免疫抑制剂(见免疫抑制部分),不会增加患皮肤癌的风险。
因此,可考虑对发展为多发性皮肤癌的移植受者改用基于西罗莫司、不含钙调磷酸酶抑制剂的免疫抑制方案。目前,没有数据表明肝移植受者患其他常见癌症(如乳腺癌,结肠癌,前列腺癌或其他癌症)的风险增加。
结果
总体而言,肝移植的结局非常好,但根据肝移植的适应症以及与供体相关的因素而有很大差异。目前,肝移植后一年的总患者生存率为88%。肝移植后五年的患者生存率为73%。

如上所述,这些结果根据肝移植的适应症而有很大差异。例如,接受肝细胞癌移植的患者一年生存率仅为86%,而接受胆道闭锁肝病移植的患者一年生存率为94%。令人鼓舞的趋势是,在过去20年中,患者短期和长期生存率持续提高。随着手术技术、器官保存、围手术期护理和免疫抑制的进步,生存率有望在未来继续提高。
这篇关于肝移植笔记9 肝移植基础知识Discussion of liver transplantation-UCSF的文章就介绍到这儿,希望我们推荐的文章对编程师们有所帮助!